FEB 2021 The Joint Committee on Vaccination and Immunisation (JCVI) has now considered the evidence for Phase 2 of the UK’s COVID-19 vaccination programme.
JCVI has been asked by the Department for Health and Social Care (DHSC) to give its advice on the optimal strategy to further reduce mortality, morbidity and hospitalisation from coronavirus (COVID-19) disease. Evidence suggests an age-based approach remains the most effective way of reducing death and hospitalisation from COVID-19.
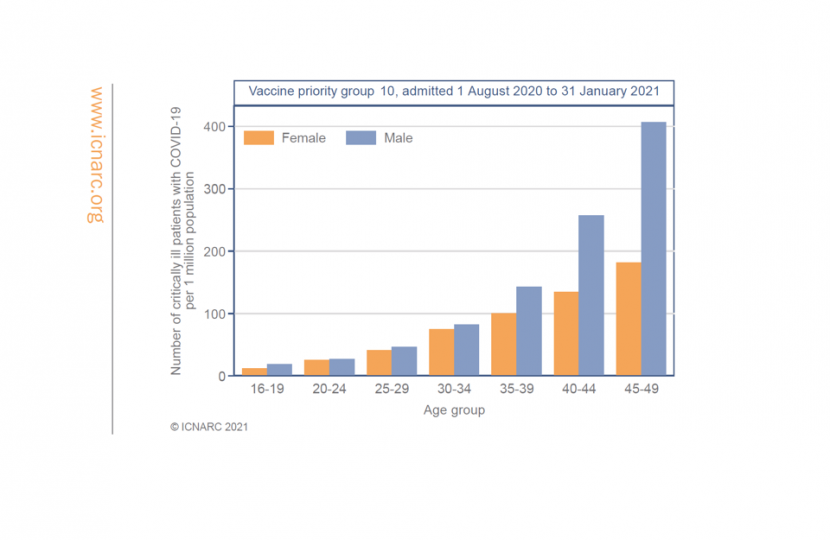
For Phase 2, modelling studies also indicate the speed of vaccine deployment is the most important factor in maximising public health benefits against severe outcomes. After groups 1 to 9 in Phase 1, people aged 40 to 49 years are at highest risk of hospitalisation, with the risk reducing the younger you are. Prioritisation will therefore continue in the following order, once all at-risk groups in Phase 1 have been offered at least one dose of the vaccine:
- all those aged 40 to 49 years
- all those aged 30 to 39 years
- all those aged 18 to 29 years
The committee agreed that mass vaccination targeting occupational groups would be more complex to deliver and may slow down the vaccine programme, leaving some more vulnerable people at higher risk unvaccinated for longer. Operationally, simple and easy-to-deliver programmes are critical for rapid deployment and high vaccine uptake. JCVI strongly advises that people promptly take up the offer of vaccination when they are offered.
Professor Wei Shen Lim, COVID-19 Chair for JCVI, said:
"Vaccinations stop people from dying and the current strategy is to prioritise those who are more likely to have severe outcomes and die from COVID-19. The evidence is clear that the risk of hospitalisation and death increases with age. The vaccination programme is a huge success and continuing the age-based rollout will provide the greatest benefit in the shortest time, including to those in occupations at a higher risk of exposure."
Dr Mary Ramsay, Head of Immunisations at Public Health England (PHE), said:
"Delivering a vaccination programme on this scale is incredibly complex and the JCVI’s advice will help us continue protecting individuals from the risk of hospitalisation at pace. The age-based approach will ensure more people are protected more quickly. It is crucial that those at higher risk – including men and BAME communities – are encouraged to take the vaccine, and that local health systems are fully engaged and reaching out to underserved communities to ensure they can access the vaccine."
Occupational exposure
While many have been able to work at home during the pandemic, some occupations are not compatible with home working and cannot be undertaken without interaction with other people. In these circumstances individuals may be exposed to SARS-CoV-2. These include workers who have public facing roles, or who work in close contact with co-workers. Commuting to a workplace using public transport constitutes a potential additional risk of infection.
JCVI has reviewed data to understand the association between occupation and the risk of exposure to SARS-CoV2, the risk of COVID-19 disease and the risk of COVID-19 related severe outcomes, including mortality.
The evidence indicates that certain occupations have a higher risk of exposure, and these are more likely to be occupations involving frequent contact with multiple other people in enclosed settings. These encompass the elementary occupations, manufacturing, processing and those working in the caring, leisure and a broad range of service occupations. Where increased risk of serious disease is evident, this is considered likely to be associated with a combination of various risk factors for exposure and poorer outcomes including: older age, an overrepresentation of certain underlying health conditions in those undertaking certain jobs, socio-economic deprivation, household size and inability to work from home. Occupational risk associated with poorer outcomes from COVID-19 has predominantly affected men aged 40 to 49 years (please see annex A for more details).
Delivery of a programme targeting occupational groups is recognised to be operationally complex given a number of key factors:
- robust data on the infection exposure risk for every occupational group, or in every occupational setting, are not available
- occupation is not routinely recorded within primary care records and these records may not be up-to-date
- advice to target certain occupations could be considered discriminatory towards those in occupations where no data are available or that are not accurately listed within primary care records
- workplaces that may be associated with higher exposures to infection may include individuals from multiple occupational groups
Overall, JCVI considers that an operationally simple, age-based programme starting with those aged 40 to 49 years is the optimal way to protect individuals, working in jobs with a potentially higher risk of exposure to SARS-CoV2, from severe disease related to COVID-19.
FAQ's
When will phrase two start?
The next phase will start as soon as the first one is over. Everyone over 50 should get their offer by 15th April, so phrase two will likely start in April.
Why haven’t any groups like shop workers/teachers/police officers been prioritised?
The JCVI did not want to single out any occupational group because of the unfairness. One of the great things about the scheme the JCVI constructed our advice around those that are risk of getting severe complications from Covid. It is overall aim to save as many lives and possible.
The JCVI think the right thing to do is to make sure that we minimise the amount of people who die, by using that by using the vaccine most effectively and age is still the predominant risk factor for severe illness or death due to Covid- more so that any risk from the work environment.
One of the many difficulties with occupational status is that it's not very well recorded or not completely recorded in primary care records- many people do not have their job on their GP records. We know the age-based programme is simple and works very well and that's why it seemed sensible to continue with that keeping an eye on speed, as speed of deployment is the important factor.
Teachers/police officers/shop workers over the age of 50 or those with underlying illnesses, will have already got the vaccine or will be getting in the coming weeks.
Did the JCVI even consider teachers to be prioritised?
Yes, the JCVI did looked at these groups very carefully and found that in terms of workplace exposure risk teachers actually have a much lower occupational exposure risk that those working in the catering industry for example. The exposure risk for teacher is relatively small because they have ventilation in classrooms. In fact, the data shows that teachers are no more likely to catch Covid at than any other member of the population who goes to work.
What about police officers?
While some police officers do sometime come into close contact with Covid-19, the ONS data on the occupations with the highest rates of death begin with restaurant and catering establishment managers/proprietors, following onto metal working & machine operatives, food/drink process operatives and chefs.
A lot of police officers work outside in a ventilated environment, a lot of police officers were behind desk with no exposure is so there are patches within each occupation. To reiterate the point any police officer over the age of 50 will be immunised and then any police officer then is between 40 & 49-year-old group will be offered the vaccine.
We know locally in Essex, many Police have already been called to take missed vaccination slots at local hospital and vaccine hubs.
What about those with a learning disability?
The JCVI has already announced those on the GP learning disability register should be prioritised for a Covid vaccine.
People with a "severe or profound" learning disability in England & Wales were already in priority group six for the coronavirus vaccine, along with unpaid carers for those with disabilities and the elderly. All adults with Down's Syndrome have already been offered a jab, in priority group 4.
The NHS is being asked to work with local authorities to identify other adults, in residential care or receiving support to live in the community, who are severely affected by a learning disability and may not be registered, but who should be offered a vaccine.
COVID-19 vaccine surveillance reports
The latest estimates from Public Health England (PHE), September 2021, indicate that the vaccination programme, delivering 79 million vaccinations in England, has directly averted over 230,800 hospitalisations, of these around 178,900 hospitalisations have been avoided in those aged 65 and over in England. It has also prevented between 23.7 and 24.1 million infections and between 119,500 and 126,800 deaths. Based on antibody testing of blood donors, 97.8% of the adult population now have antibodies to COVID-19 from either infection or vaccination.
Several studies have estimated vaccine effectiveness against hospitalisation in older people. They indicate high levels of protection with all vaccines against the Alpha variant and over 90% effective against hospitalisation from the Delta variant among all 3 vaccines. In most groups, there is relatively limited waning of protection against hospitalisation for at least 5 months after the second dose.
Since the beginning of the programme, Public Health England (PHE) has been monitoring the effectiveness of the vaccines in the real world as set out in the COVID-19 vaccine surveillance strategy and the impact on:
- symptomatic disease
- hospitalisation
- death
- infection (symptomatic or asymptomatic)
- transmission
Below is PHE’s weekly COVID-19 vaccine surveillance report (20 May 2021 – week 20). The table below summarises the evidence we have to date on vaccine effectiveness against different outcomes.

To view the full report, please visit: https://www.gov.uk/government/publications/covid-19-vaccine-surveillance-report
First Rollout FAQ's
Who gets the vaccine first? /When will I get my vaccine? (March 2021)
The independent Joint Committee on Vaccination and Immunisation advises the Government on which vaccines we should use, and what the priority groups are. Their decision is based on a range of factors, including the different characteristics of different types of vaccines, to work out the most effective way to protect as many people as possible and save as many lives as we can, using the best available clinical, modelling and epidemiological data. The top four most vulnerable groups account for 88% of COVID deaths.
The NHS target for vaccinating top 4 priority groups was January to mid February & the NHS met the target and has now offered a vaccine to everyone in the top four priority groups. This covers around 32 million people, these groups are:
- ✓ Residents in a care home for older adults and their carers
- ✓ All those aged 80 and over. Frontline health and social care workers
- ✓ All those aged 75 and over
- ✓ All those aged 70 and over. Clinically extremely vulnerable individuals
- ✓ All those aged 65 and over
- ✓ All individuals aged 16-64 with underlying health conditions which put them at higher risk of serious disease and mortality
- ✓ All those aged 60 and over
- ✓ All those aged 55 and over
- ✓ All those aged 50 and over
Are there regional differences in supply or are sites running out of vaccine?
- Vaccines are being distributed fairly across the UK to ensure the most vulnerable are immunised first and all GPs will continue to receive deliveries as planned. The NHS, government and armed forces are doing everything we can to vaccinate those most at risk as quickly as possible.
- Parts of the country have made very significant progress and gone faster than the average. We’re putting more supply into areas that have more to do, with the NHS doing brilliantly to deliver the amount of supply we have.
- Up to 2,000 people working in roles crucial to the continuity of the COVID-19 vaccine supply chain will be offered jabs to help ensure the UK gets the doses it needs to protect the most vulnerable
- The vaccine rollout is a huge logistical operation and there are a number of reasons why the rate of progress is different across the country. Some of the discrepancy will be due to differing population levels as some areas have a greater percentage of over 80’s (one of the highest-priority groups).
- It also takes time to set up the vaccination sites, because each site must be approved in terms of safety and accessibly. The Primary Care Network is made up of all the local GPs working together and the local Clinical Commissioning Group’s helps set up the GP led sites. So, setting up these sites needs the co-operation and agreement of the all the local Doctors and the administrators.
- Staffing is another important issue. In areas where there are high Covid cases, like in London and the East of England, appear to be hampered more by staff shortages due to infection and self-isolation.
- Other reasons include the storage, delivery and rate of production of the vaccine. The first vaccine to be approved- the Pfizer/BioNTech vaccine- must be kept at around -70C (-100F). This super cold storage is usually found in hospitals. However, the Oxford University/AstraZeneca vaccine is much more easily transported and stored. It can be sent to vaccination centres in refrigerated vans or cool boxes and stored in special vaccine fridges, normally found in GP practices between 2C to 8C, whilst also protected from light. Some areas started getting the vaccine first because they had the facilities to store the Pfizer/BioNTech vaccine first. Now the Oxford University/AstraZeneca vaccine has been approved the NHS will be able to reach more places and more people.
The NHS is expanding the vaccine programme literally every week and while some places in the UK are ahead of the target pace, please be assure the NHS is still on track to meet their targets.
Why did some parts of the UK been vaccinating the over 70s before finishing vaccinating the over 80s?
In some areas of the NHS system, there have been instances of the over 70s receiving their vaccine before the over 80s age group – in line with the national policy. This would happen if there were no further people aged over 80 booked for a vaccination on a particular day or if we had a surplus supply of vaccine. If this instance occurred, people in the next age group would be invited in order to ensure no wastage of the vaccine. Moving towards this more flexible approach across the first four cohorts will support our achievement of a vaccination offer to all priority individuals by mid February. It will also reduce inequality of access and maximise pace.
Will people with a learning disability receive greater priority?
The Joint Committee on Vaccination and Immunisation (JCVI) has announced that those on the GP learning disability register should be prioritised for a Covid vaccine.
People with a "severe or profound" learning disability in England & Wales were already in priority group six for the coronavirus vaccine, along with unpaid carers for those with disabilities and the elderly. All adults with Down's Syndrome have already been offered a jab, in priority group 4. The NHS is being asked to work with local authorities to identify other adults, in residential care or receiving support to live in the community, who are severely affected by a learning disability and may not be registered, but who should be offered a vaccine.
I have received a text message – is it a scam?
If you have received a text message from Basildon University Hospital it means that you are eligible to have the COVID-19 vaccine during the first wave of the vaccination programme. The text you have received will have clear NHS Mid and South Essex (MSE) branding with a link that allows you to book an appointment and there will also be a telephone line option. If you are concerned that the message is a scam, please call 01245 515 919.
You may also get a phone call from the NHS Immunisation Management Service. This call will be from 0300 561 0240. This will be a reminder to book your COVID-19 vaccination appointments. The person you speak to will see if you need any help and support. If you already have appointments booked, you can: view your appointments, cancel your appointments or book appointments again HERE
If you are in one of the eligible groups, live in Essex and need further help to book an appointment, you can ring the Helpline on 0344 2573 961 (open 9am-4pm, local rate).
I’ve received a letter but someone I live who is the same age hasn’t yet. Can we get vaccinated together?
If you have received a letter and live with someone who is also eligible but has not received a letter, it is likely that theirs will follow shortly. If you both in the are in the top priority groups. You can book at the same time by contacting the NHS to book in your jab. The easiest way is to do this is through the NHS National Booking Service, or if you can’t get online then you can call 119 or you can speak to your local GP practice.
How do I arrange an appointment for my 2nd dose?
The NHS in Essex wants to make sure residents know what to do when it’s time for their 2nd dose of the vaccine. The 1st dose of the COVID-19 vaccine should give you good protection from coronavirus. But you need to have the 2 doses of the vaccine to give you longer lasting protection. It’s important that the same vaccine is used for both doses and it will help if you return to the same place as where you had your 1st dose. Please remember that until you have had your second dose, you should continue to follow all the guidance including social distancing, wearing face coverings and hand washing
Where did you receive your 1st dose? / Where should you have your 2nd dose ?
- If you received your first dose at a GP-led vaccination service: you should return there for your second dose, your GP may have already given you a date, if you don’t have a date yet, your GP will contact you soon.
- If you received your first dose at a large vaccination centre: you should already have been given a date to return there for your second dose If you don’t have a date yet, you can book one online using the National Booking System or by calling 119. If you need help, please ring the local helpline: 0344 2573 961 (open 10am to 4pm).
- If you received your first dose at a hospital: If you had your first dose at Basildon Hospital, Broomfield Hospital, Orsett Hospital, Southend Hospital or Towngate Theatre in Basildon and booked your appointment online using ShiftPartner, then your second appointment must be also booked using ShiftPartner. If you need to change the date of your second appointment, you can do this online using ShiftPartner. If you need help please call the Mid & South Essex COVID-19 Vaccination booking line on 01245 515919 (only queries about second dose). If you booked your first dose by calling the Mid and South Essex COVID-19 Vaccination Booking Line, they will be in contact with you.
- If you received your first dose at a community pharmacy: you should have already been given a date to return there for your second dose. If you don’t have a date yet, you can book one online using the National Booking System or by calling 119.
When the 2nd dose will be given?
The latest evidence suggests the 1st dose of the COVID-19 vaccine provides protection for most people for up to 3 months. As a result of this evidence, when you can have the 2nd dose has changed. This is also to make sure as many people can have the vaccine as possible. The 2nd dose was previously 21 days after having the 1st dose, but has now changed to 12 weeks after. If you:
- have already had your 1st dose and are due to have your 2nd dose before Monday 4 January, keep your appointment
- have already had your 1st dose and are due to have your 2nd dose after Monday 4 January, the NHS will contact you about when you’ll have your 2nd dose
- are due to have your 1st dose after Wednesday 30 December, you’ll be given your 2nd dose 12 weeks later
Why has the dosage schedule for vaccines been changed?
The four UK Chief Medical Officers agree with JCVI advice that prioritising the first doses of vaccine for as many people as possible on the priority list will protect the greatest number of at-risk people overall in the shortest possible time. The decision we have taken will literally double the number of people who are protected over the next few crucial months. Everyone will still receive a second dose within 12 weeks of their first.
The MHRA has approved a longer gap between doses for both the AstraZeneca vaccine and the Pfizer vaccine. The latter has concerned some people. Specifically many are citing a figure of 52% for protection after the first dose.
To clarify, the 52% figure is the average protection over these 21 days, so it includes that initial time before the immune system has had time to create a response. If one instead looks at the day 10 to day 22 period one instead gets an efficacy value of 86% (there will be confidence intervals around that). Whereas if one looks at the day 0 to day 10 period there is an efficacy of 10%. The 52% figure is a combination of those two completely different scenarios. It's not useful. People shouldn't be citing it in this context.
For any more information explaining the 52% figure mentioned above, please visit: https://threadreaderapp.com/thread/1344347380917940226.html?fbclid=IwAR1CpwyYhLBILcadtKNy2AUvd2fbLVL9-ZdutSvBSPrqo3LjwpJCKdHaYFs.
Can I have the vaccine if I am of childbearing age, pregnant or breastfeeding? (Updated 16 April 2021)

There’s no evidence the COVID-19 vaccine is unsafe if you’re pregnant or breastfeeding. The JCVI has advised that pregnant women and women who are breastfeeding should be offered the COVID-19 vaccine at the same time as the rest of the population, based on their age and clinical risk group. There have been no specific safety concerns identified with any brand of coronavirus (COVID-19) vaccines in relation to pregnancy.
Real-world data from the United States shows that around 90,000 pregnant women have been vaccinated, mainly with mRNA vaccines including Pfizer-BioNTech and Moderna, without any safety concerns being raised. Based on this data, the JCVI advises that it’s preferable for pregnant women in the UK to be offered the Pfizer-BioNTech or Moderna vaccines where available. There is no evidence to suggest that other vaccines are unsafe for pregnant women, but more research is needed.
The advice, published in Public Health England’s Green Book, a clinical professional guide for vaccinators in the UK, still advises that pregnant women should discuss the risks and benefits of vaccination with their clinician, including the latest evidence on safety and which vaccines they should receive. If you have any concerns, speak to a healthcare professional before having the vaccination. More info: http://nhs.uk/CovidVaccine.
The greatest risk factor for severe outcomes from COVID-19 is age, which is why pregnant women should be invited for vaccination along with their age or clinical risk group. Women who are planning pregnancy, are in the immediate postpartum, or are breastfeeding can be vaccinated with any vaccine, depending on their age and clinical risk group.
The JCVI will continue to closely monitor the evidence on COVID-19 vaccination in pregnancy and will update its advice as required.
For more information on the JCVI’s new advice on COVID-19 vaccination for pregnant women, please visit: https://www.gov.uk/government/news/jcvi-issues-new-advice-on-covid-19-vaccination-for-pregnant-women. You can also view the updated guidance in the ‘COVID-19: the green book, chapter 14a’, coronavirus (COVID-19) vaccination information for public health professionals, at: https://www.gov.uk/government/publications/covid-19-the-green-book-chapter-14a.
How do I spot a scam?

The COVID-19 vaccine is free of charge on the NHS. The NHS will never ask for:
- your bank account or card details
- your pin or banking password
- copies of personal documents to prove your identity such as your passport, driving licence, bills or payslips